Deep Vein Thrombosis – “insidious foe”
It is estimated that 16–20 thousand people in Hungary develop deep vein thrombosis each year, and several thousand die from its complications – even though thrombosis and its dangerous complication, pulmonary embolism, could be avoided! I write here about this “insidious foe”, deep vein thrombosis. What exactly does deep vein thrombosis mean? When blood "clots" in one of your veins and a blood clot (so-called thrombus) forms, then […]
It is estimated that 16–20 thousand people in Hungary develop deep vein thrombosis each year, and several thousand die from its complications – even though thrombosis and its dangerous complication, pulmonary embolism, could be prevented! I write here about this “insidious foe”, deep vein thrombosis.
What exactly is deep vein thrombosis?
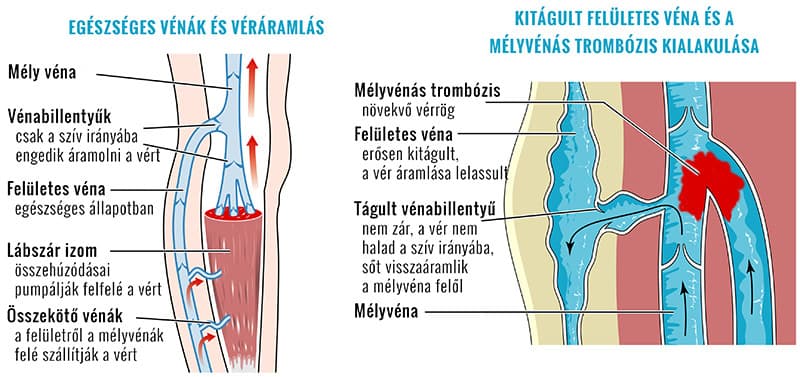
When blood "clots" in one of your veins and a blood clot (a so‑called thrombus) forms, we speak of thrombosis. There are two forms: one affecting the superficially running veins and one affecting the deep veins. Superficial vein thrombosis is milder, often can be borne on the leg and may resolve on its own. However, deep vein thrombosis requires great attention because it can have severe, life‑threatening consequences!
A thrombus that forms in a deep vein adheres to the vein wall and grows. If a fragment breaks off, the bloodstream can carry it to the heart and from there to the lungs. This is called a pulmonary embolism. The blood clot blocks one of the lung arteries. The consequence depends on the size of the clot. A large clot can immediately lead to a severe, life‑threatening condition. Occlusion of a major pulmonary artery can cause sudden death.
Veins form a network throughout your body. They collect used blood and return it to your heart, from where it picks up fresh oxygen in the lungs. Your arteries carry it back to your organs. Superficial veins, as the name suggests, collect and carry blood from the skin, mucous membranes and areas close to the body surface. They turn inward and join the larger deep veins, which ultimately run toward the heart.
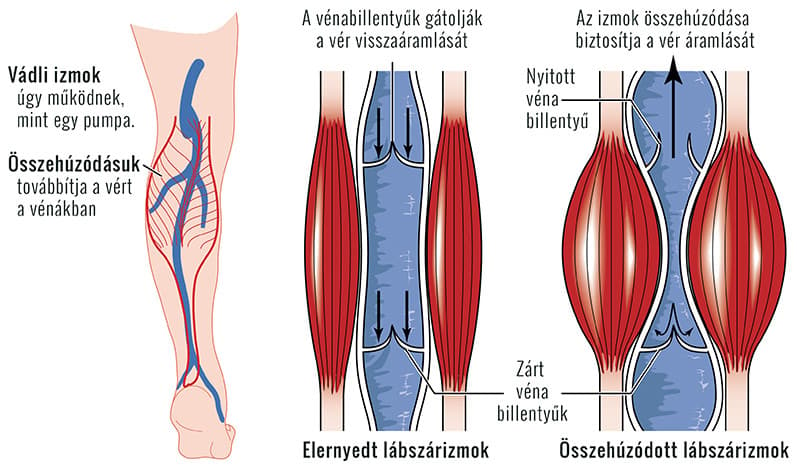
Blood flows passively in your veins. When you move, your muscles contract, compress the veins, and squeeze the blood out of them. The blood always moves toward the heart because valves in the veins act like gates or locks, allowing flow only in that direction.
Potential causes of deep vein thrombosis
There are many predisposing factors for deep vein thrombosis – none of them alone necessarily leads straight to the disease, but the presence of several factors together increases the risk significantly.
- injury to the vessel wall,
- changes or slowing of blood flow,
- changes in the composition of the blood, increased tendency to clot.
The risk factors for deep vein thrombosis can include the following:
- Prolonged immobility: if you do not move your legs for a long time, blood flow slows and your blood may clot. Prolonged bed rest, for example due to a fractured limb in a cast, or a hospital stay after surgery can cause this.
- Even long periods of sitting can be dangerous: for example, during long drives or flights, if you do not use your legs for extended periods, venous blood can become "stagnant" in your legs.
- Injury to or surgery on the veins can increase the risk of clot formation; general anesthesia may also dilate the veins, which can contribute to this outcome.
- Pregnancy increases the pressure on the pelvic and leg veins.
- Some cancers cause an increase in substances that promote blood clotting in the body.
- Heart failure means the heart does not pump blood as effectively as needed, so blood flow slows.
- A pacemaker or a central venous catheter can irritate the vessel wall and slow blood flow.
- Oral contraceptives can increase the blood's tendency to clot and thus raise the risk of deep vein thrombosis.
- Smoking strongly affects blood clotting and circulation.
- Severe obesity also adversely affects blood circulation.
- If you have previously had deep vein thrombosis or a pulmonary embolism, you are more likely to experience a recurrence.
- In addition, inherited clotting disorders or a family history of previous deep vein thrombosis and pulmonary embolism can play a major role in the disease's development.
Warning signs
Deep vein thrombosis often develops insidiously and without obvious signs – in most cases there are no marked early symptoms. However, if you experience the following set of symptoms, seek medical attention immediately (with as little movement as possible):
- swelling of your ankle, foot, or lower leg,
- severe pain in the same area,
- the skin becomes red and feels warm to the touch.
What to do if symptoms appear
It is important that acute treatment of deep vein thrombosis can only and exclusively take place in a hospital, where specialists intervene with anticoagulant and circulation‑improving medications. During this time there is little you can do yourself.
After discharge from the hospital, take your anticoagulant medications exactly as prescribed, attend follow‑up appointments, and you have two further tasks: alleviate residual symptoms and prevent recurrence!
Fortunately, medical technology is also "on your side." Several types of devices that can be used safely at home can help with this.