ECG – what you need to know about the electrocardiographic examination
I have written before that one important sign of how your body works is its electrical activity. Body processes are controlled by electrical impulses, so the functioning of your brain and your heart is largely governed by electricity. Electrocardiography records the electrical activity of your heart; it is performed with an ECG (electrocardiograph) device.
The ECG is one of the most frequently performed medical diagnostic tests. It is used for the rapid detection of heart problems and for monitoring the condition of your heart. An ECG device is considered basic equipment in every clinic and in ambulances alike.
Today some personal electronic devices, such as smartwatches, also offer ECG monitoring functions. It is important to know that these gadgets are not diagnostic tools and are only truly helpful in detecting certain rhythm disturbances.
The need for an ECG is usually decided by your treating physician, and the recording is made at their request.
Why do we use ECG?
It is a non-invasive (i.e., performed without entering the body), painless procedure. A diagnostically valid recording lasts 10 seconds. The entire examination, including undressing, placing the electrodes, recording and redressing, takes only a few minutes.
It is suitable for diagnosing disturbances in the heart's electrical activity and circulation at any age. For example, it can detect:
- cardiac rhythm disturbances (arrhythmias) – there are many different types
- chest pain (angina pectoris)
- detection of blocked or narrowed coronary arteries (coronary artery disease)
- immediate detection of an acute heart attack (myocardial infarction)
- retrospective recognition of a previous heart attack
- monitoring treatments, for example the function of a pacemaker or the effectiveness of medications.
When might an ECG be needed?
An examination is usually carried out if you experience any of the following signs or symptoms:
- chest pain
- dizziness, forgetfulness or confusion
- palpitations
- rapid or very fast pulse
- shortness of breath
- weakness, fatigue or loss/reduction of movement ability in certain body parts.
An electrocardiographic examination is generally unnecessary in situations where the risk of any heart problem is low, especially in people without symptoms. For example, knee pain is obviously unrelated to the heart, so no ECG will be performed for that.
If heart disease is common in your family (parents, siblings), regular ECG screening is recommended, even if you have no symptoms.
Long-term ECG recording
I mentioned above that the standard ECG records the heart's electrical activity for 10 seconds. Most heart-related complaints are persistent, meaning they can be detected immediately, even with a single recording.
However, there are rhythm or circulation disturbances that appear and then disappear shortly after. By the time you arrive at the clinic, the ECG may only capture the returned normal state.
If your symptoms turn on and off regularly, long-term ECG recording may be necessary.
- Holter device: a small, portable device that continuously records the heart's electrical signals. It is usually worn for 24 or 48 hours. On average you have 80–120 thousand heartbeats in a day; it records each and every one.
The device itself does not analyze the data, it only records. Analysis takes place when you return the unit to the clinic and the data are read out. Doctors use computer assistance to search for abnormalities and hidden problems. - Event monitor: this portable device is similar to a Holter monitor.
The main difference is that the device does not record continuously but continuously analyzes signals from your heart and starts recording when it detects an abnormality.
Because of the smaller storage capacity, such a device consumes less power and is therefore suitable for longer examinations than a Holter monitor. An examination can last 7–30 days.
In addition to automatic operation, you can press a button to start recording if you feel symptoms.
Risks
The ECG (electrocardiographic) examination is completely harmless and safe. There is no risk of electric shock because the device does not send electrical energy into your body. On the contrary, the electrodes placed on your body record the heart's electrical activity.
When the electrodes are removed, you may feel something like the removal of a larger adhesive bandage.
If suction electrodes are used (which remain on your skin with the help of vacuum), a "suction mark" may appear at the electrode site, which is a result of local blood engorgement. It disappears within a few minutes.
In people with thin skin, fragile capillaries or bleeding disorders, prolonged suction may even cause bruising. This is not dangerous but can be unpleasant. If you are aware of such a condition, inform the person performing the examination and ask them to use self-adhesive electrodes instead of suction electrodes.
Self-adhesive electrodes are also more hygienic than suction electrodes that are placed one after another on multiple patients. In our country they are rarely used because they are more expensive than suction cups.
With sensitive skin, some people may develop redness under the electrode. This indicates an allergy to one of the components of the gel or adhesive used in the electrode. When the electrode is removed, the rash disappears shortly afterward.
How to prepare for an ECG?
No preparation is required for a routine ECG.
Inform the staff about your medications and dietary supplements – these can influence the results of the test.
Mention if you have contact allergy to self-adhesive electrodes or if suction cups have caused bruising for you before.
How is the examination performed?
The examination is most often carried out in a medical office or examination room. Usually an ECG technician or another professional performs it. In certain cases your family doctor or an emergency physician may perform it at your home.
Preparation
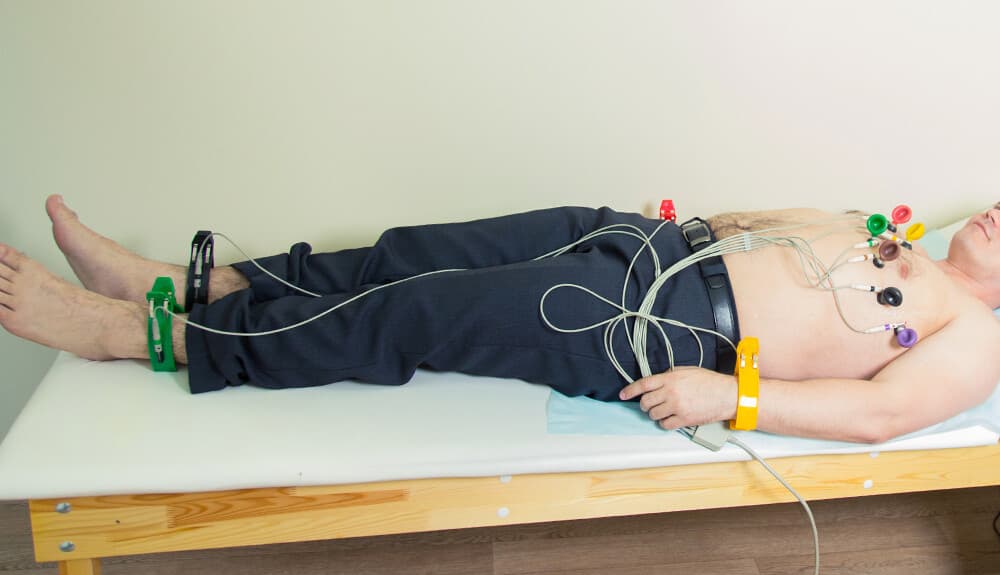
The person performing the test may inform you about what will happen. You will be asked to remove your shoes, socks or stockings. Take off your outer clothing, including your bra. Remove necklaces and watches.
When you are ready, you will be asked to lie on an examination couch.
For an ECG recording the electrodes are always placed on the same spots on every person. Therefore, if there is dense hair where the electrodes go, it must be shaved off. Electrodes placed incorrectly because of "hair saving" can distort the ECG and lead to false results. It is therefore in your interest to allow hair removal.
During the examination
During a standard ECG test, four sensing electrodes connect to your limbs (on ankles and wrists). In addition, six electrodes are placed on your chest from right to left. In some special cases, three additional electrodes may be placed on your back (along the spine) so the test can be done sitting rather than lying down.
The electrodes are connected by wires to the electrocardiograph, i.e., the ECG device. It records the electrical signals generated by your heartbeats.
The computer inside the device processes the information and displays curves on the monitor or records them on paper.
Breathe normally during the test. Lie comfortably and try to keep your muscles relaxed. Movement, talking or trembling during the examination can distort the results. If you feel cold, ask for a blanket.
A standard ECG test takes only a few minutes from start to finish.
After the examination
The ECG recording does not affect your body's functioning in any way, so no special rest or restriction is required afterward. You may continue your daily activities as usual.
Results
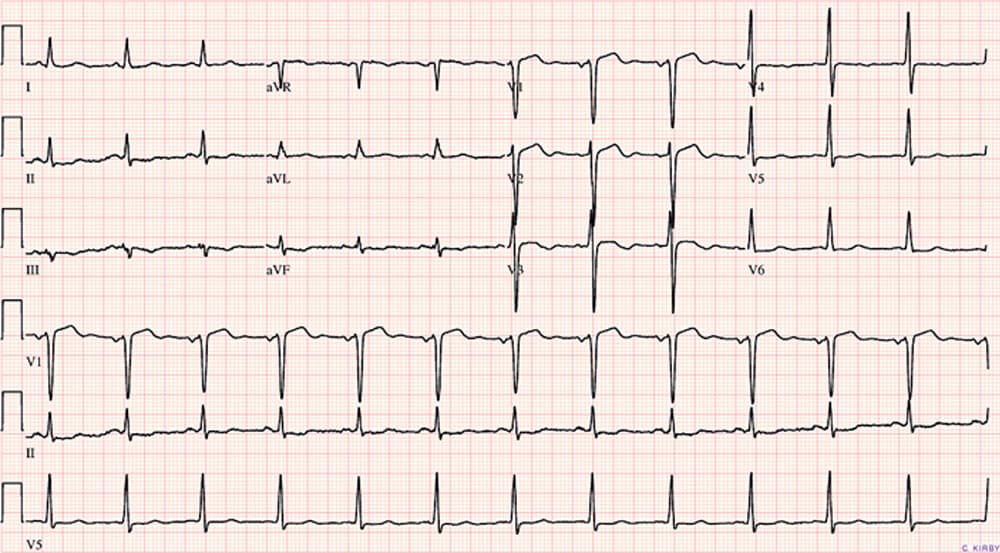
An ECG recording typically looks like this. The many waves may not mean much to you, but to an experienced physician they often reveal the problem at a glance. Sometimes a few minutes of analysis and measurement are needed. Thus the result may be communicated to you a few minutes after the test.
If the electrocardiogram is normal, no further cardiac investigations are usually necessary.
If the results show abnormalities, repeated ECGs or other diagnostic tests may be needed, such as laboratory tests, chest X-ray or echocardiography. Treatment will depend on what is causing your symptoms.
What does the doctor look for on the ECG?
To a physician the ECG trace is a treasure trove of information. In the evaluation they primarily pay attention to the following aspects:
Heart rate
Heart rate can be detected and counted by feeling your wrist or the carotid arteries.
The ECG shows your heartbeats even when the pulse cannot be felt, for example when a thick layer of fat "hides" it or when it is too fast or irregular to be counted accurately.
In such cases the recording can still accurately identify unusually high heart rate (tachycardia) or low heart rate (bradycardia).
Heart rhythm
The ECG is excellent at detecting cardiac rhythm disturbances (arrhythmias). In the figure above you can see at a glance that the waves (individual heart contractions) appear rhythmically, regularly, at equal intervals. In arrhythmia this regularity is disrupted and rhythm errors become immediately visible.
Arrhythmias are caused by malfunctions of the heart's electrical system. In addition, certain medications (for example beta-blockers), cocaine, amphetamines, and over-the-counter cold and allergy medicines can also trigger arrhythmias.
Structural abnormalities
The size (height) of the ECG leads and their relative proportions indicate enlargement of the heart's chambers or walls, congenital heart defects and other heart problems. Based on these ECG signs further tests (chest X-ray, echocardiography, etc.) may be ordered.
The heart's blood and oxygen supply
ECG examinations are most often performed because of chest pain. The physician looks for ECG signs of oxygen deprivation in the heart muscle. When the myocardium does not receive sufficient blood, the heart muscle cells become oxygen-starved, causing intense chest complaints (angina pectoris, i.e., tight chest pain).
Oxygen deprivation causes changes on the ECG trace and even indicates which area of the heart is affected.
Based on the ECG and symptoms, further tests may be necessary to determine whether the blood supply disturbance is transient (unstable angina) or sustained (heart attack, myocardial infarction). The former can sometimes be treated with medications, while the latter requires immediate intensive care and intervention.
Heart attack
A previous or ongoing heart attack (myocardial infarction) produces characteristic changes on the ECG, which can serve as proof.
Which of the 12 leads shows the infarct-related change immediately informs the physician which region of the myocardium is affected—for example the anterior, posterior or inferior wall, or the interventricular septum. It also provides information about the extent of the damage (the size of the area that has died).
If the physician detects any abnormality on the ECG (electrocardiogram), further investigations may be ordered before starting treatment.


