Ganglion – benign cyst
A ganglion cyst is a lump that appears on the hand or foot and is often painful. Despite its alarming appearance, it is usually nothing to fear because it is benign. Due to the symptoms and the disturbing appearance, patients most often choose removal surgery. Postoperative rehabilitation plays a key role in restoring movement. I write now about the important things you should know.
A ganglion cyst is a lump that appears on the hand or foot and is often painful. Despite its alarming appearance, it is usually nothing to fear because it is benign. Due to the symptoms and the disturbing appearance, patients most often choose removal surgery. Postoperative rehabilitation plays a key role in restoring movement. I write now about the important things you should know.
What is a ganglion?
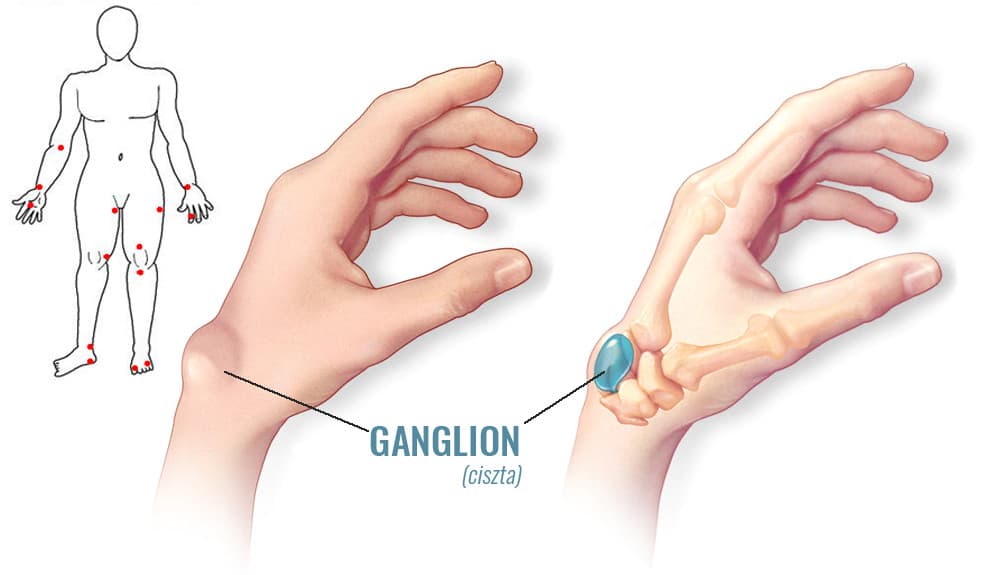
A ganglion is a benign cyst filled with fluid or a gelatinous material. It presents as a swelling or lump on the hand or foot, characteristically around joints and tendons.
Its size ranges from that of a pea to a walnut and can change over time.
In most cases ganglion cysts are painful, especially at the beginning. The intensity of pain does not correlate with size. Certain movements or external pressure (from a tool or object) can trigger it.
The cyst is benign and harmless, but frequent pain and its cosmetic appearance (a noticeable, attention-drawing lump) are bothersome for the patient.
In severe cases the large size of the cyst and its connection with the joint can hinder movement, or it may press on vessels and nerves, causing sensory disturbances.
How does a ganglion cyst form?
A ganglion is a bulging of the joint capsule or the tendon sheath — in a sense a "hernia".
Joint fluid is pushed through and accumulates in the ganglion. Increasing pressure in the cyst closes off the pathway for the fluid to return. That is, the cyst cannot empty. If for some reason this does happen, the cyst can resolve on its own.
A ganglion most commonly appears on the dorsal (back) side of the wrist and around the finger joints. About 85% of cysts are found near the wrist joint and 10% near the foot and ankle. On the wrist they are most common above the scaphoid and lunate bones (os scaphoideum and os lunatum).
They generally appear spontaneously without any particular cause. They can affect anyone, but are three times more common in women than in men. They mostly occur in young adults and are rare in children. In older age there may be an association with joint inflammations (osteoarthritis).
The exact cause is unknown; trauma, degenerative processes, or overproduction of synovial fluid are suspected.
Diagnosis
Diagnosis is usually straightforward because the location and feel are characteristic. An experienced physician often recognizes it at first glance and confirms it by palpation.
Ultrasound examination is generally sufficient. It clearly shows the fluid in the cyst and also differentiates it from other conditions (lipoma, Dupuytren's contracture and similar).
If there is uncertainty or before removal to thoroughly map its position, an MRI can be performed. This shows its relationship to tendons, the joint, and nearby vessels and nerves.
Before MRI became widespread, it was common to inject contrast into the cyst and take an X-ray to outline the entire cavity and its connection to the joint capsule. With MRI examinations this invasive method is slowly falling out of use.
Treatment of the ganglion
Medical data show that 40–55% of ganglia can resolve spontaneously without treatment.
An invasive method is aspiration of the ganglion. The surgeon inserts a needle into the lump (sometimes ultrasound-guided) and withdraws the cyst content with a syringe. A small amount of steroid (anti-inflammatory) is then injected into the site. The method has immediate effect, but a high recurrence rate. Aspiration gives the best results for ganglia of the flexor tendons of the hand.
Surgical removal remains the "gold standard" — it is considered the most effective method for treating ganglion cysts. During the operation the surgeon excises the entire ganglion complex, including the cyst, its stalk, and a portion of the adjacent joint capsule.

After surgery the wrist is immobilized with a splint so it is not moved for a few days. Immobilizing wrist movement is important because otherwise motions could pump joint fluid from the joint capsule into the cyst site and surrounding tissues, leading to adhesions and restricted motion.
The role of physiotherapy
A ganglion cyst cannot be eliminated by any home medical device. I have already discussed the possibilities for that.
However, physiotherapeutic methods play a major role in postoperative recovery and in restoring joint mobility.
During surgical excision — as mentioned — not only is the ganglion removed but also part of the joint capsule or tendon sheath from which it arose. These incisions heal with a scar. The scar can cause adhesions and tethering. Prolonged postoperative immobilization increases this undesirable phenomenon — but it is necessary to prevent recurrence.
After ganglion surgery it is common that, once the splint is removed, the joint does not move fully or only partially because of adhesions.
Scar healing can be stimulated with softlaser treatment started from the day after surgery. Treating the scar with an acupuncture softlaser (e.g. Personal Laser L400) promotes the production of an appropriate amount of collagen. As a result, the scar becomes even, thin and strong. Without treatment less collagen and more connective tissue forms, so the scar becomes thick, red and raised, increasing the likelihood of adhesions.
Great emphasis must also be placed on physiotherapy. However, this can begin only after the splint is removed. Professional massage also helps to release adhesions.
The goal of physiotherapy is to restore normal use of the hand. Ask a physiotherapist to teach you the exercises to do at home!
Two to three weeks after ganglion surgery you should already be able to use your hand with full range of motion. If not… then something was missed in the rehabilitation… go back to your surgeon and ask for advice.
Patients who receive appropriate postoperative care have lower recurrence rates and faster recovery.