Thrombosis – when your vein is blocked
Thrombosis most often develops in your leg, particularly in the lower leg. It often represents a life-threatening condition! According to data, it affects 16–20 thousand people annually in Hungary and several thousand die from its complications.
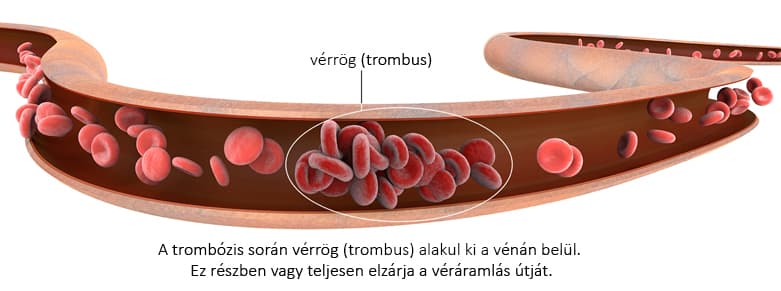
Thrombosis is the "clotting" of blood within a vessel. A blood clot (medically called a thrombus) forms and acts like a plug that entirely or partially blocks the vein. As a result, blood cannot continue flowing toward the heart, causing increasing, tense pain and swelling.
Types of thrombosis
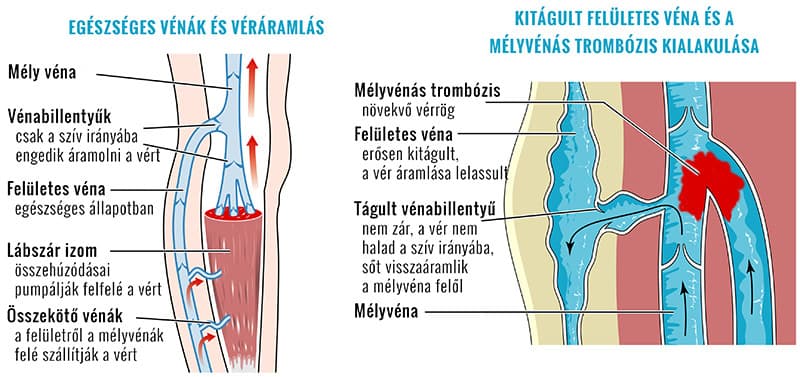
- Superficial. In this case the clot forms in veins running close to the skin surface. Superficial venous thrombosis is milder, often can be managed at home and usually resolves on its own.
- Deep vein. In deep vein thrombosis the clot forms in vessels running deep between the muscles. This is serious and can have life-threatening consequences!
Causes of thrombosis
Several predisposing factors are known. The risk is higher if more than one is present.
- injury to the vessel wall
- changes or slowing of blood flow
- changes in blood composition, increased tendency to clot
Risk factors
Risk factors for developing thrombosis may include:
- Prolonged "forced rest". Extended bed rest, such as after surgery or immobilization due to a fracture and casting: the muscles do not pump venous blood, flow slows and the blood can clot.
- Prolonged sitting. Sitting for hours in a car or on a long flight can be dangerous. Immobility causes circulation in the legs to stagnate and blood may clot. That is why you should regularly stop, stand up and exercise your legs during travel.
- Vein injury or surgery. These can increase the risk of clot formation. During general anesthesia veins dilate – during long surgeries the risk of clot formation is higher.
- Cancer – in some forms the amount of substances that promote clotting increases. Thrombosis may also occur if a growing tumor compresses nearby veins.
- Inherited clotting disorder
- Heart failure. In this case the weakened heart pumps blood more slowly than needed, so blood flow slows.
- Pace-maker or a central venous catheter can irritate the vessel wall and slow blood flow.
- Birth control pills can increase the blood's tendency to clot.
- Smoking greatly affects clotting and circulation.
- Pregnancy – although not an illness, the growing fetus can compress the pelvic and leg veins, slowing their circulation.
- Severe obesity adversely affects circulation.
- Previous thrombosis. Those who have had deep vein thrombosis previously have a higher chance of recurrence.
The first symptoms of thrombosis
Thrombosis often develops insidiously and unnoticed. In most cases there are no clear early warning signs. The disease usually begins with:
- swelling of your ankle, foot or lower leg;
- severe pain in the affected area;
- the skin becomes red and the swollen area feels warm.
What to do if you suspect thrombosis
If you notice the above symptoms, seek medical attention immediately!
Once the thrombosis process has started, there is little you can do at home; delaying will only worsen the situation.
The treatment of acute deep vein thrombosis must take place only in a hospital, where specialists treat you with anticoagulant and circulation-improving medications, or even with catheter-based interventions.
Complications of thrombosis
A serious complication can be pulmonary embolism
Fortunately it develops in only some cases.
If the blood clot (thrombus) formed in a vein moves from its place or a fragment breaks off, it is carried by the bloodstream to the heart and then to the lungs – this process is called embolization. A clot that reaches the lung is called a pulmonary embolus.
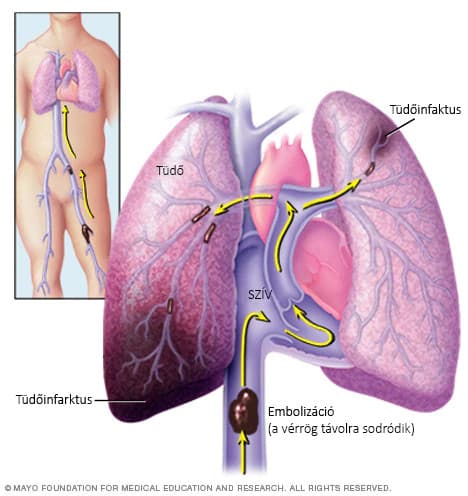
Depending on its size, the clot blocks one of the lung's arteries, creating a sudden, severe, life-threatening condition. Occlusion of a larger pulmonary vessel often causes immediate death; a smaller embolus leads to the death of the affected lung tissue (pulmonary infarction) and always heals with consequences.
Post-thrombotic condition (post-thrombotic syndrome).
A resolved thrombosis unfortunately always leaves a "residual condition" that you must live with for the rest of your life.
If you have successfully passed the acute phase, what happens next largely depends on you.
The management of symptoms left by thrombosis and the prevention of recurrence cannot be done by anyone for you. Every day, continuously, you have to "take care" of it yourself.


