Urinary incontinence and its treatment
Hundreds of thousands of people in our country struggle with difficulties in holding urine. Most patient information sites recommend pads, diapers, medications and surgeries as “solutions”, but these bring no or only minimal improvement. Better results come from strengthening the pelvic floor muscles or relearning how to relax them. Various pelvic floor exercise routines can be effective in half to one year (provided you practice 40–50 minutes daily). With electrical incontinence stimulators the process is significantly faster. A beneficial effect can be felt after just 2–3 weeks of treatment. Within three months stress, urge and mixed incontinence can be completely eliminated or at least significantly improved in almost all cases.
What incontinence means
Incontinence is the phenomenon when you cannot hold back urine and/or stool. In such cases urine or stool drips, leaves a mark on your underwear and you cannot stop it voluntarily (even though you were able to before). It can develop at any age and becomes more frequent with advancing age.
Urine leakage is almost as common as hay fever, affecting about 6–7% of people, yet it is almost taboo and rarely talked about. Still, there is a solution in most cases! Fecal incontinence is less common.
It is more common among women, but men can be affected too. Men’s pelvic floor muscles are stronger and less open, making them less vulnerable; their urethra is roughly 15 cm longer and they do not give birth. Male incontinence is most often related to prostate problems.
Incontinence
- is not a natural consequence of childbirth or aging
- may have easily treatable causes but can also indicate a more serious disease, so see a doctor first for an examination
- can lead to complications, skin problems and infections
- makes commuting to work, your relationship and your sex life more difficult
- can cause shame, anxiety and even depression, which may lead to social withdrawal and isolation.
Types of incontinence
The simplest way to classify urinary problems is by their underlying cause.
Stress incontinence
In this case the pelvic floor muscles and the muscles that close the urethral opening weaken and closing pressure decreases. You notice that a few drops of urine escape when you cough, sneeze, blow your nose, bend over, step down from a stair, or lift a heavier object. This is most common among young and middle-aged women.
Weakening of the urinary sphincter is often caused by injuries sustained during childbirth, especially if an episiotomy is performed. During menopause estrogen deficiency can also reduce tissue elasticity. Stress incontinence can also be a “civilization harm” caused by prolonged sitting (at work, while traveling or in front of the TV) and a sedentary lifestyle. Pelvic floor muscle tone decreases, they no longer support the bladder properly and do not close it adequately.
In men it often appears after prostate surgery, especially if the urethra or the neck of the bladder is damaged.
Obesity worsens the condition in both sexes, since the visceral fat increases the burden on the bladder and supporting muscles.
Symptoms usually worsen gradually: at first they appear only with increased abdominal pressure, later with minimal strain such as walking. In the most severe form, leakage can occur even at rest.
In stress incontinence strengthening the pelvic floor muscles can eliminate the symptoms. Pelvic floor exercises (which may take months to show results) or the much more effective muscle stimulation (which can yield results in a few weeks) can be used.
Urge incontinence
In this form the need to urinate appears suddenly and very intensely, making it almost impossible to suppress. You have difficulty controlling the passage of urine voluntarily. This is caused by increased tension, hypersensitivity and overactivity of the bladder muscle.
Transient urge incontinence can be caused by stressful situations, for example exam or pre-meeting tension. Your bladder “wants to help”, producing an urgent need to urinate.
It is common in older patients because with age the holding strength of the sphincter muscles also deteriorates. Other causes may include stroke, cerebral atherosclerosis, Parkinson’s disease, multiple sclerosis, etc. In men, prostate enlargement can trigger such symptoms.
Treatment for urge incontinence involves relaxing the bladder muscle and retraining correct activity, as well as increasing sphincter strength. This can be achieved by applying appropriate muscle stimulation impulses.
Mixed incontinence
Incontinence is mixed when both forms are present, i.e. weakness of the pelvic floor muscles and increased bladder activity are observed.
Treating mixed incontinence requires combined muscle stimulation. On the one hand, sphincter strength must be increased, and on the other hand bladder muscle tension must be reduced. Appropriate muscle stimulation impulses can provide this.
Transient incontinence
Transient urinary incontinence can be caused by dietary habits or certain medications.
- Several alcoholic drinks are diuretic—beer, wine and various spirits. Consuming them in quantity leads to rapid bladder filling and urgent need to urinate.
- Caffeine—like alcohol—causes rapid bladder filling and reduces storage capacity.
- Carbonated soft drinks, coffee, tea, artificial sweeteners and citrus fruits increase bladder activity.
- Some medications, such as tranquilizers, sleeping pills, antihypertensives and heart medicines, can also affect bladder regulation.
Fecal incontinence
In this case you cannot hold stool. You can read details here: Fecal incontinence and its treatment
Treatment of incontinence
Tens of millions of people worldwide struggle with urinary retention difficulties, and in our country this problem affects roughly eight hundred thousand people.
Most patient information sites suggest pads and diapers as a “solution.” However, these do not produce any improvement since they only serve to absorb urine. They are not intended to improve the underlying problem.
Incontinence pad
Almost every article dealing with urinary problems mentions the incontinence pad (also called incontinence underwear or diaper pants) as an important tool in treating incontinence.
However, mentioning the incontinence pad like this is simply a big deception.
The pad absorbs dripping urine and stool, but it has no effect on the problem itself. Incontinence will not improve at all from wearing it—not even a little. No matter how long you wear the diaper, you will never get rid of urine leakage because of it.
It may be necessary, but don’t expect improvement from it alone! Look for other, more effective methods!
Behavioral therapy
Create a schedule in which you intentionally empty your bladder and bowels regularly. If you know the problem becomes critical after more than 2 hours, go to the toilet deliberately every 90 minutes.
Surgical treatment for incontinence
Surgical interventions mostly do little for recovery and only provide a temporary solution. Muscles and ligaments shortened and “tightened” by surgery will stretch again within 1–2 years and the problem begins anew.
The solution is strengthening the pelvic floor muscles and reducing bladder activity.
Almost every method has limitations. Some only reduce symptoms and do not affect the underlying cause. I believe that a combination of methods gives the best result.
Pelvic floor exercises (Kegel exercises)
Daily pelvic floor exercises performed for 40–50 minutes aim to voluntarily tighten and relax your pelvic floor muscles. The drawback is that results develop very slowly and require months of training. Although pelvic floor exercises are the cheapest and simplest home treatment for incontinence, they are also the slowest.
Effectiveness can be significantly improved with electrical treatments.
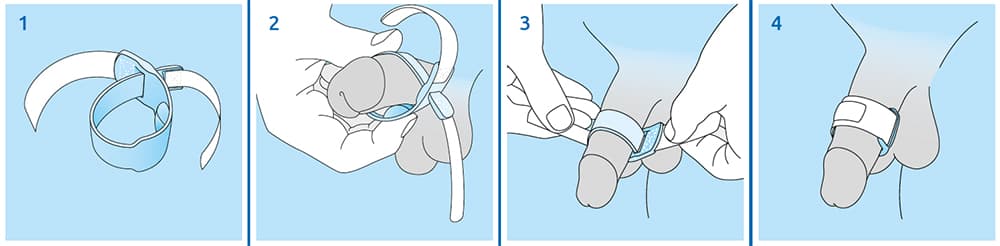
Prosecca strap
Many men suffer from incontinence; even mild urine leakage strongly affects quality of life.
The Prosecca strap is a very simple yet effective solution for urine dribbling. Placed on the penis, pressure on the urethra stops urine leakage. It can be worn "invisibly", comfortably and discreetly.
Usage: The Prosecca strap must be placed on the penis. The slightly raised pressure pad should be positioned in the middle on the underside of the penis (along the course of the urethra) and the strap tightened. Tighten it as much as possible without causing pain. Fasten the Velcro and the leakage stops.
Electrotherapy and biofeedback
Biofeedback
A biofeedback device uses a sensor probe placed in the vagina (or in the anus for men) to support pelvic floor exercises. It detects the muscle's electrical activity (EMG) when the muscle contracts. It provides feedback—by number or light—about contraction intensity.
The biofeedback device itself does not treat; it helps you learn the most effective execution of the exercises. With biofeedback you can achieve results faster and more effectively than with pelvic floor exercises alone.
FES, that is functional electrical stimulation
In this case a device assists the training of the pelvic floor sphincter muscles via an intracavitary electrode placed in the vagina (or in the anus for men), directly treating the pelvic floor muscles. It is a passive method, meaning it treats without you having to do anything.
With muscle stimulation both muscle weakness and excessive muscle activity can be treated—of course different programs are needed for strengthening and different ones for relaxation. Stimulation helps even when incontinence is caused by injury to the motor nerve running to the sphincter or other problems, so you may not be able to perform voluntary exercises.
Another advantage of the method is “training” the nerves that run to the sphincter. In a hyperactive sphincter, stimulation causes the muscle to relax and it “learns” the relaxed state.
The stimulator device is easy to use and you can safely perform this intimate treatment at home without the presence of a doctor.
Stimulation produces results significantly faster than pelvic floor exercises. With regular daily treatment the muscles strengthen/relax and control over stool holding and emptying is regained. The first results can be noticed after 2–3 weeks, but treatment should be continued for 8–10 weeks. The result achieved then should be maintained with a sustaining regimen, for example regular pelvic floor exercises or 1–2 stimulations per week. (If you stop treatments entirely, the problem may return over time.)
Suitable devices can be the Biolito or the evoStim UG
Click here for guidance on performing stimulator treatment for incontinence.
ETS device
The most modern and effective incontinence treatment device is the ETS, that is biofeedback-triggered muscle stimulation treatment.
A probe placed in the vagina (or in the anus for men) senses when you voluntarily contract the pelvic floor muscles. At a preset "squeeze" strength the device “assists” by delivering a stimulation impulse through the probe to strengthen the sphincter. This makes the muscle contraction more effective.
The ETS, i.e. combined biofeedback + stimulator device, provides the most effective method of treating incontinence.
The evoStim E or the EvoStim P devices are suitable for such treatment.
Incontinence treatment devices
Stress, urge and mixed incontinence can be treated with several methods. Muscle stimulation is one of the most effective among them. A beneficial effect can be felt after 2–3 weeks of treatment and with persistent therapy it often completely eliminates or at least significantly reduces symptoms.
Electrical treatment cannot be performed for everyone
In some cases electrotherapy is not recommended, for example the presence of a pacemaker or severe cardiac arrhythmia. Here you can read detailed information about the contraindications of electrostimulation.
The article Practical incontinence stimulator treatment teaches the basics of functional stimulation treatment.
People often ask whether success is guaranteed. No. There is no single medical method that produces complete improvement for everyone.
Most cases are successful, meaning symptoms are significantly reduced or completely disappear.
If you follow medical advice, adhere to usage rules and perform the treatment regularly, you will most likely experience a beneficial effect. You may notice the first signs after just 2–3 weeks of treatment. With persistent electrotherapy you can reach a state in 2–3 months that can be considered a lasting result. After that you can switch to maintenance treatment (1–2 sessions weekly) to preserve muscle strength.
"a little biology"
Your body disposes of excess water and certain substances with the help of the kidneys. Urine then passes into the bladder, which can store about 300–400 ml. Urine leaves the body through the urethra. Closing and opening the urethra is partly voluntary. When the bladder fills, it “sends a message” to your brain—this triggers the urge to urinate. If you are able to control urination you can decide whether to void immediately or hold it. If bladder tension exceeds a certain level, you can no longer hold it voluntarily and it empties reflexively (in plain language, you wet yourself).



