Uterine prolapse and its treatment
Female urinary incontinence (involuntary leakage of urine) is often caused by bladder prolapse or uterine prolapse. The bladder or uterus is displaced from its normal position, descends downward and presses on the pelvic floor muscles. This can cause a constant uncomfortable sensation, make sexual intercourse painful, and disrupt urinary and bowel continence. Its treatment is much more difficult than that of “simple” incontinence.
Female urinary incontinence (involuntary leakage of urine) is often caused by bladder prolapse or uterine prolapse. The bladder or uterus is displaced from its normal position, descends downward and presses on the pelvic floor muscles. This can cause a constant uncomfortable sensation, make sexual intercourse painful, and disrupt urinary and bowel continence. Its treatment is much more difficult than that of “simple” incontinence.
A bit of anatomy
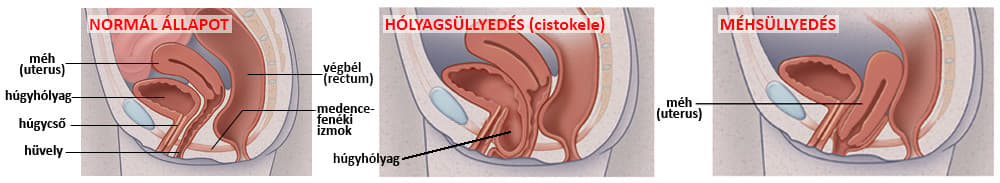
The uterus and the bladder are located in the pelvic cavity. The bladder lies in front and below. Behind it is the vagina, and above the vagina is the uterus. Posterior to the vagina are the rectum and the anal opening.
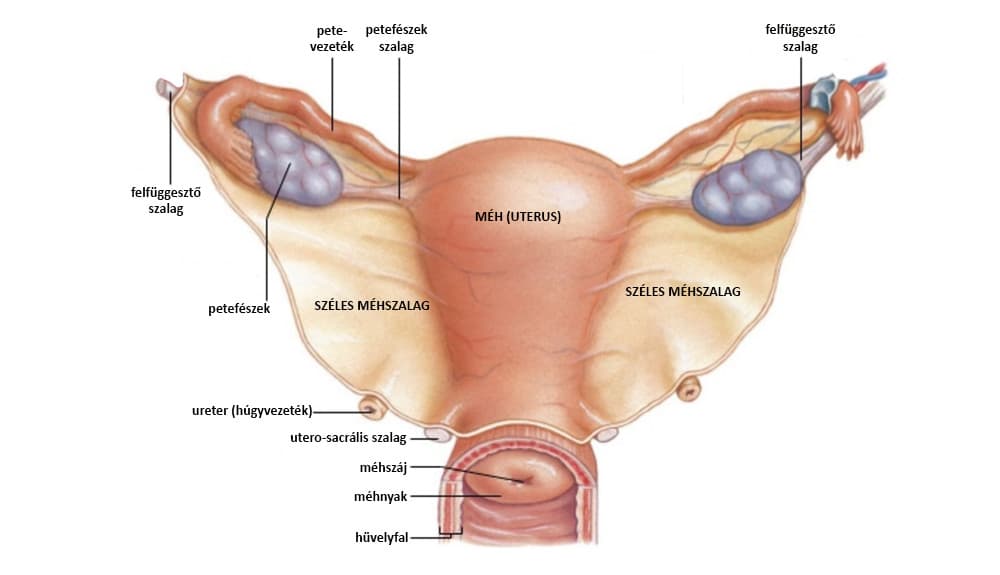
The bladder and the uterus are covered from above by the peritoneum, which also helps anchor them into the pelvis. In addition, the uterus is fixed by ligaments to the pelvic structures and the sacrum. Think of it like a chandelier hung from the ceiling by wires or straps.
The uterus sits at the "top" of the vagina; the cervix protrudes slightly into the upper part of the vagina. The vagina itself is flexible but not rigid, so it contributes to support only to a limited extent.
The pelvic floor muscles lie about 10–15 cm below the uterus. They form a closure plate at the base of the pelvis and prevent the abdominal organs, including the uterus and bladder, from slipping downward.
Some parts of the pelvic floor muscles encircle the anal opening and the urethra like a ring. These sphincter muscles ensure urine and stool continence.
Bladder prolapse and uterine prolapse
Uterine prolapse (prolapsus uteri) occurs when the suspensory ligaments become stretched and lose their support. Because the ligaments are longer, the uterus descends lower in the pelvic cavity.
As a result, the cervix first bulges into the upper part of the vagina from above.
In bladder prolapse (prolapsus vesicae urinariae), the posterior part of the bladder sags and bulges into the vagina.
What causes it?
Mainly weakening of the pelvic floor muscles and supporting tissues, which may be caused by:
- Injury to ligaments and pelvic floor muscles during pregnancy, difficult labor, or childbirth.
- Being overweight: fat accumulates not only under the skin but also between the abdominal organs (in the mesentery), creating a thick fat layer that acts as a weight on the intestines and internal organs and tends to pull them downward.
- Lower estrogen levels after menopause.
- Chronic constipation or straining during bowel movements.
- Chronic cough or bronchitis.
- Repeated heavy lifting.
- Lack of physical activity and poor posture due to prolonged sitting can worsen the condition or even cause it. These lead to weakening and stretching of the pelvic floor muscles, reducing their supportive strength.
Symptoms
In mild cases, bladder or uterine descent may cause no symptoms. Later you may notice the following (usually not all at once):
- An uncomfortable sensation in the vagina, pelvis, lower abdomen, groin or lower back. Often a dragging pain that worsens during sexual intercourse or menstruation.
- A feeling of pressure or a "weight", as if something is "about to fall out of your vagina".
- On self-examination or during hygiene you may feel a bulge inside the vagina.
- In severe cases, the mucosa or even the cervix may protrude from the vagina. This can dry out, chafe, itch or develop small sores that may bleed.
- Urine may leak, especially when lifting, coughing or sneezing.
- Frequent urge to urinate.
- Recurrent urinary tract infections because the bladder cannot fully empty.
- Difficulty with bowel movements.
- Painful sexual intercourse. You may notice involuntary urine leakage during sex, or even difficulty achieving orgasm.
Diagnosis
By self-examination you may feel that your vagina has shortened or that something is pushing in from the front or above. In bladder prolapse the lower and middle parts of the vagina, anteriorly, show a palpable or visible bulge of the bladder. In uterine prolapse the upper part of the vagina will show a downward movement of the cervix that can be felt.
Most often your gynecologist notices it during a routine exam or during a vaginal inspection (colposcopy) performed as part of screening.
Imaging methods such as ultrasound or MRI can confirm the diagnosis, but they are usually not necessary because the condition is clear on examination.
Treatment
Treatment of uterine and bladder prolapse is twofold.
On the one hand, the aim is to improve support by strengthening the pelvic floor muscles. Because strengthening muscles takes time, the effect develops over 2–3 months with daily training, so modern devices allow you to perform the treatments at home. This means you don't have to visit the clinic every day.
In severe cases the uterus or bladder is surgically repositioned using gynecologic reconstructive surgery. With surgical laser methods without cutting the elastic fibres of the vaginal wall are stimulated to strengthen and improve support. In invasive procedures (laparoscopic or open abdominal surgery) the uterus is often secured with a ligament-like support which is sutured to the pelvic bone or other structures to pull it back into place.
There are several methods to strengthen the pelvic floor muscles.
vaginal weights
Various medical objects placed in the vagina (cone, cube, Fleur-balls, etc.) also strengthen the pelvic floor muscles by being retained. To prevent them from slipping out you contract the pelvic floor muscles, thereby exercising them. The correct size device is prescribed by your doctor.
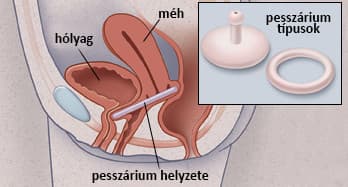
special pessary
A ring-shaped, flexible device placed in the upper part of the vagina (although called a pessary, it is different from the one used for contraception). A pessary helps support the uterus and bladder and can prevent them from descending into the vagina. You can remove and clean a pessary and, after a little practice, easily reinsert it yourself.
pelvic floor exercises (Kegel exercises)
These are exercise routines where you deliberately contract your pelvic floor muscles. Results are expected after months of regular training. Practicing 2–3 times daily for 30 minutes is optimal. Pelvic floor exercises are the cheapest and simplest method, but also the slowest and least effective.
biofeedback
A device that, using a sensor probe placed in the vagina or anal canal, assists with pelvic floor exercises. The device senses muscle contractions and provides feedback, for example with numbers or lights indicating contraction strength. The biofeedback unit does not treat by itself but helps you learn how to perform the exercises most effectively. With biofeedback you can achieve results faster and more effectively than with exercises alone.
FES, i.e. functional electrical stimulation
A device trains the pelvic floor sphincter muscles for you. Via an electrode placed in the vagina or anal canal, the pelvic floor muscles are directly stimulated. The muscles contract and relax in response to the stimulation, which has a training effect similar to exercise. Stimulation treatment is significantly more effective than voluntary pelvic floor exercises, so it produces results faster. Still, 8–10 weeks of treatment are required. After that you can switch to maintenance treatment (1–2 sessions per week) to keep the effect. (If you stop treatment completely, the muscles will weaken again over time and the problem may return.)
biofeedback + FES (functional stimulation)
The most modern and effective — and also the most expensive — home device combines biofeedback and functional stimulation. A probe placed in the vagina or anal canal senses when you voluntarily contract the muscles, and the stimulator then "assists", making the contraction more effective. The combined biofeedback + stimulator device is the most effective home-based method for treating incontinence.
Incontinence treatment devices
Stress, urge and mixed forms of incontinence can be treated in several ways. Muscle stimulation is one of the most effective methods. A beneficial effect can be felt after 2–3 weeks of treatment, and persistent therapy often completely eliminates or at least significantly reduces symptoms.
Is the effect of stimulation guaranteed?
In mild cases, yes; in moderate and severe cases, no.
It is certain that appropriately long and intense stimulation strengthens the pelvic floor muscles. This effect alone may solve the problem in mild uterine or bladder prolapse.
In moderate and severe cases, if the uterus or bladder is already palpable at the vaginal opening or even prolapsed outside, stimulation will produce only some improvement. This is unlikely to be enough to make you completely symptom-free.
This is because the uterus is kept mainly in place by the suspensory ligaments above it, not by the pelvic floor muscles located 10–15 cm below. Just as a chandelier is not supported by the floor but by the cord hanging from the ceiling, the uterus is supported from above.
If the uterus or bladder has fully descended, stimulation alone will not help. You do not prop up a fallen chandelier from below with poles to put it back in place; you shorten the hanging cord. Similarly, a severely prolapsed uterus cannot be pushed back from below — surgical correction of the suspensory ligaments (whether laser, laparoscopic or open surgery) is usually required.
If uterine or bladder prolapse is detected early, stimulation can achieve complete symptom relief. The improved condition can be maintained with regular physical activity, exercises, weight loss and giving up a sedentary lifestyle.