Compression therapy unit — what is it for, how to choose?
Pressure therapy devices provide treatment for people with lymphatic and circulatory disorders, effectively reducing swelling and the tight, painful sensation.
In Hungary the compression therapy unit is known under several names — pressure-, wave- or pneumatic compression therapy device — but they all refer to the same device. It can be used in medical offices, in cosmetic and beauty practice, and for home treatment. In this article I write what you should know before buying a compression therapy unit.
The Hungarian term “nyirokmasszázs gép” (literally lymph massage machine) is misleading because the device is not only applicable to patients with lymphatic disease but to many conditions! For example lipedema (fat edema), venous insufficiency, pregnancy-related varicose complaints, post-thrombotic syndrome, limb swelling after stroke, improving muscle regeneration, and wellness applications.
What is compression therapy for?
Compression therapy, and within it the machine-based compression therapy — also called pneumatic compression therapy — is a treatment method particularly useful for lymphedema and many other vascular-origin circulation problems.
The compression therapy unit improves lymph flow in the lymphatic system and helps drain excess fluid from tissues. This reduces edema and the degree of swelling.
The treatment acts not only on the lymphatic system but also assists blood circulation, which can be especially beneficial in venous insufficiency.
A compression therapy unit is not meant to strongly knead muscles and therefore does not replace a sports masseur! If you want deep, strong pressure on your muscles, see a masseur. The compression therapy unit is intended to assist and improve blood and lymph circulation, so pressures of about 60–80 mmHg maximum should be used.
What is a compression therapy unit?
The compression therapy unit is essentially a medical air compressor. The pressure can be regulated very precisely to meet medical treatment needs.
Various treatment cuffs can be attached to it; the device pumps air into the cuffs' airchambers. Individual airchambers can be inflated separately, one by one, or together. The inflated airchamber creates the desired effect by compressing the tissues and thereby inducing movement and redirection of blood and lymph.
How to choose the right configuration for you?
You need to make several decisions.
- Which compression therapy unit?
- Which cuffs do you need and in what sizes?
- Do you need any additional accessories?
1. Which compression therapy unit should you choose?
You always need a device, so first decide which compression therapy unit you will buy.
Main differences between devices
- intended use
- the number of treated airchambers
- programmability and fineness of pressure control
1. Intended use.
There are units designed for home use and those intended for institutional/clinic use.
Clinics treating lymphedema generally use robust devices built for continuous all-day operation. Because maximum precision is needed in such treatment settings, clinic units use cuffs with 6, 8 or 12 airchambers. These high-end devices can cost one-and-a-half to two million HUF (Power Q-8120). Clinic assistants are familiar with these devices and often tell patients that only 6–12 airchamber cuffs are adequate. But that is not always true!
For home use, simpler devices designed for daily 1–2 hours of operation, lightweight and generally with 4 airchambers, are recommended. Such units are available in the roughly HUF 150,000–300,000 range, including necessary accessories.
Another important factor is the severity of your condition.
If your symptoms are mild and you have no complications (no wounds or ulcers), the simple and inexpensive devices are sufficient (Power Q-1000 Plus and Power Q-2200). In addition, inexpensive, simple devices are easy to operate, making them usable for older people and those less comfortable with technology. For them, even the simplest device is better than leaving edema untreated.
Significant overweight, moderately severe or severe edema, or ulcerative complications mean that the basic devices' capabilities are not enough. In such cases I recommend devices that offer multiple setting options and higher treatment precision (for example Power Q-2200 or Power Q-1000 Premium). You should also choose such a unit if you have heart disease, high blood pressure, or arrhythmia, because precise pressure-controlled treatment is very important then.
One more difference: device weight.
Four airchamber devices designed for home use weigh 2–3 kg and can be taken on a trip.
Devices with 6–12 or more airchambers are significantly larger and often weigh 10 kg or more.
2. Number of airchambers
The number of airchambers in a treatment cuff matters for treatment precision. The more airchambers a cuff has, the more finely the lymph flow can be guided. More precise treatment often achieves results in a shorter treatment time.
However, the price of the device and cuffs rises steeply with the number of airchambers, and the device's operation and setup become more complex. If you can afford it, choose the device with as many airchambers as possible (Power Q-8120).
I am convinced, however, that for everyday home treatment a 4-airchamber device is perfectly adequate for most patients.
3. Programmability
Device programs are controlled by a pressure sensor. The compressor pumps air into an airchamber and when it reaches the set pressure it stops and starts inflating the next chamber.
The simplest home devices (Power Q-1000 Plus) generally provide a single “program”: the cuff chambers are inflated from bottom to top (for a leg cuff: first the chamber at the foot/ankle, then the calf, then the knee, then the thigh). Pressure is the same in every airchamber. On such a device you can only set treatment pressure and duration. These simple devices can be successfully used for mild edema, varicose complaints, and post-thrombotic conditions.
If your edema is more severe and long-standing, refills quickly, or has complications (weeping, ulcer), a basic device is only a very compromised solution. If you can afford it, choose a higher-spec device. They are more effective but also more expensive.
Mid-range compression therapy units (Power Q-2200) already offer several inflation programs, although the same pressure is still set for all airchambers in the cuff.
The most effective units allow setting different pressures for each airchamber of the treatment cuff, adjusting the pressure-hold time, and the resting time between inflation cycles. Medical studies show that lymphedema treatment is more effective when pressures are higher in the lower airchambers and decrease going upward. It is similarly important that the pressure-hold time can be set so that one cycle lasts at least 45 seconds.
Higher-quality devices can set different pressures for each airchamber (Power Q-1000 Premium).
This feature is especially important for treating the lower limbs. Treatment is more effective if a pressure gradient can be set — higher pressure at the foot and lower pressure upward — so lymph can flow upward faster.
In addition, on a more precise unit (Power Q-1000 Premium) the pressure-hold time is adjustable. When an airchamber reaches the set pressure, the unit holds that pressure for a set duration, so the compression lasts longer and lymph displacement is more effective. Thus a device that allows adjusting pressure-hold time provides more effective treatment.
2. Treatment cuffs
Another important thing is selecting the correct treatment cuffs.
You obviously need to obtain cuffs that suit your problem. Lymphedema can affect different areas and individual body shape and size also influence the choice.
If your arm is edematous, you should get an arm cuff in the right size. For leg and trunk treatment there are different cuffs.
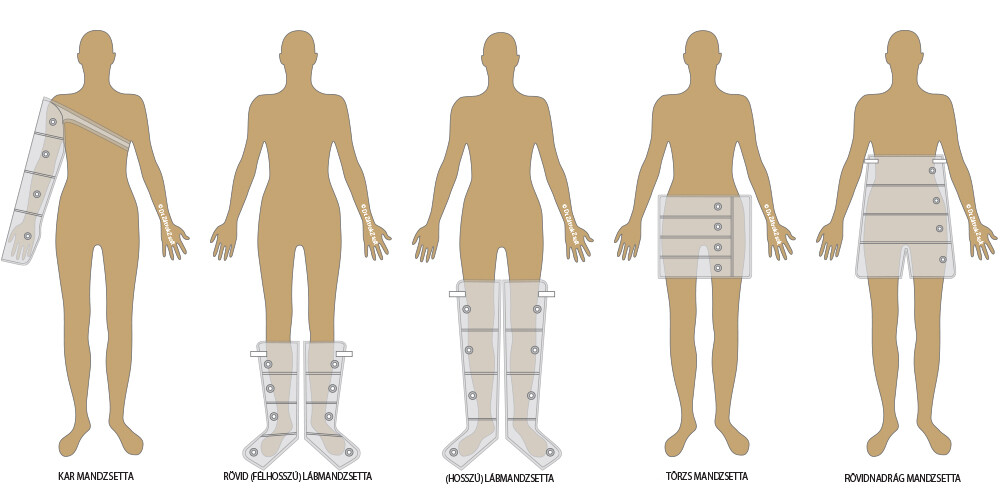
Most manufacturers offer arm, leg, waist and pant cuffs for the devices, and multiple sizes are available.
The illustration shows the variety of cuffs that can be chosen — of course not every manufacturer offers all of them.
Choose the right size for you! Measure your circumferences and compare them with the size chart.
Arm cuff
Arm lymphedema is usually unilateral, so you may only need one cuff. If you buy the device as an athlete to improve muscle regeneration, consider purchasing two arm cuffs so you can treat both arms simultaneously. The arm cuff has a Velcro strap so it can be secured under the opposite armpit.
Below-knee (half-length) leg cuff
This roughly knee-length cuff is specifically for treating post-thrombotic syndrome. It can be used 3–4 months after thrombosis to treat residual effects. For lymphedema this cuff is only suitable if swelling is limited to the foot and at most the ankle. If it extends higher, a long leg cuff is necessary.
Thigh-length leg cuff
This cuff is excellent for leg lymphedema, venous disease, and post-thrombotic conditions. For athletes it helps muscle regeneration. Depending on whether one or both legs are affected, you can buy a single cuff or a pair. If the “standard” sizes are not suitable, expanders can increase the size.
Waist cuff
Buy this if your lymphedema extends up to the thigh. In that case, the trunk should be treated as well. The cuff is wrapped like a belt, starting where the top of the thigh cuff sits. It can also be used for cellulite treatment — although the pant cuff is more effective for that.
Pant cuff
This is effective for treating the upper thigh, buttock area and lower abdominal region. It is an optimal complement for beauty treatments, especially for cellulite treatment or after cavitation.
How often can machine compression therapy be applied?
Machine compression therapy should be used as needed. That means you should treat as soon as you feel tightness or swelling.
If you wait until the swelling is pronounced and the limb is very tight, it will be much harder to reduce it!
Depending on how quickly the swelling refills, you can treat several times a day! Usually 20–30 minutes per session is enough and the total daily treatment time on the same limb should not exceed 120 minutes.
Shorter, more frequent sessions are recommended rather than one long session.
Appropriate treatment pressure
I have written before: the compression therapy unit is intended to improve blood and lymph circulation. Compression therapy does not replace sports massage, so you must not set strong, painful pressure. The aim is to improve and stimulate venous and lymphatic circulation; low pressure is required.
Most medical studies indicate that compression therapy can be performed sufficiently with pressures between 40 and 60 mmHg. Obviously, the lower the pressure you apply, the longer it will take to achieve the effect. (If you drive a car at 60 km/h you arrive slower than at 120 km/h.)
Using high pressures above 100 mmHg will worsen your condition and can eventually make the lymphedema untreatable!
Moreover, very high pressure can strain your heart, so be particularly careful if you have heart disease or high blood pressure — pressures below 60 mmHg are recommended. This lower pressure is still effective in lymphedema!
If your unit allows it, set the cuff pressures so that the lower airchamber has the highest pressure and it decreases upward. For a 4-airchamber cuff, for example, set 60-50-50-40 mmHg (foot – calf – knee – thigh), while for a 6-airchamber cuff set 60-60-50-50-40-40 mmHg per airchamber.
Treatment time per session should be 20–30 minutes. Generally, reduction of swelling can be achieved in 10–15 days.
However, this does not mean you can stop treating! Swelling will return, so you will likely need to use the compression therapy unit for life, daily. This is how you can keep swelling suppressed and avoid constant symptoms.
Recommended treatment pressure ranges
The purpose of using a compression therapy unit is to improve blood and lymph circulation, which does not require high pressure; high pressure is actually harmful. Perform treatments according to your treating physician or therapist's instructions. If you did not receive specific guidance, follow these general treatment guidelines.
| Condition | pressure (mmHg) | Treatment time (min) | Cuff |
| Arm lymphedema | 30-60 | 20-30 | Arm cuff |
| Leg lymphedema | 30-60 | 20-30 | Leg, trunk, pant cuff |
| Lipedema (fat edema) | 50-85 | 30-40 | Leg, pant cuff |
| Venous insufficiency | 40-50 | 30 | Leg, below-knee cuff |
| “Heavy legs” | 40-50 | 30 | Leg, below-knee cuff |
| Varicose ulcer | 30-50 | 40-60 | Leg, below-knee cuff |
| Post-thrombotic condition | 50-60 | 50-60 | Leg, below-knee cuff |
| Muscle regeneration after training | 80-90 | 20-30 | Leg, pant cuff, arm cuff |
Frequently asked questions
When is machine compression therapy not usable?
Machine compression therapy is contraindicated in some cases, and in other cases treatment must be performed with greater caution and at lower pressures.
It must never be used on a limb or body part with an acute deep vein thrombosis. External pressure can dislodge the clot and cause a potentially fatal pulmonary embolism.
In bacterial or fungal skin infections, massage can spread the pathogens and worsen the infection.
In heart failure, post-heart attack state, cardiomyopathy and in patients with persistently high blood pressure despite treatment, machine compression therapy may be used with great caution. In these cases never use more than one cuff at a time; treat only one region at once. Although this takes more time, the additional fluid returned to the circulation will not overly burden the heart, so risk is not increased. Also limit treatment pressure to 40–50 mmHg and use longer sessions at lower pressure.
I have an old single-chamber compression device. Can I use it to treat lymphedema?
First-generation compression devices inflated the entire cuff at once and then deflated it. They were initially adopted as a basic lymphedema treatment. However, it soon became clear that simultaneous full inflation produces excessive pressure and, in congenital lymphedema, could in some cases lead to damage of lymphatic vessels and nodes over years. Therefore lymphedema therapists specifically prohibit using old-type pumps.
Modern devices inflate the cuff sequentially rather than all at once. Cuff pressure is very precisely controllable and can be adapted to the patient’s condition. Use a modern device!
My therapist says machine compression is forbidden. Is that true?
There is no single drug, device or method that works the same for every patient!
There have always been clinicians, therapists and patients who did not get a good result with the device and therefore do not recommend its use. But for every unsuccessful case there are hundreds of very good results. Machines are not suitable for everyone and successful treatment depends on using a precise device and the correct settings.
Incorrect settings can cause harm (too high pressure) or be ineffective (too simple a device, too short treatment time, etc.).
THE KEY IS A HIGH-QUALITY DEVICE AND PROPERLY SET TREATMENT!
My therapist says the machine does not start lymph flow and even worsens edema.
That statement is not correct in this form. As mentioned above, poorly set treatment can cause complications, while correctly adapted settings to the patient’s condition do not cause harm.
A recent medical textbook (Evidence-based Physiotherapy, Tamás Bender, 2017) states that there are no medical data proving the efficacy of manual lymphatic drainage; it persists largely from tradition.
In contrast, numerous studies confirm the effectiveness of machine-based therapy.
In my opinion there is no single “guaranteed” method. Machine compression therapy alone can reduce symptoms by 60–70%. Other measures are also needed: bandaging and wearing compression stockings, therapist-performed manual lymph drainage, self-massage, etc. This article of mine discusses home treatment options.
Each of these adds a few percent of effectiveness. The more methods you apply, the closer you get to your normal circumference.
I do not find it acceptable that a therapist bans a potentially helpful treatment based on incorrect or partial information. If lymphedema is not treated properly, the patient suffers the consequences.
The facts show that compression therapy units can effectively reduce symptoms and that incorrect information can unsettle patients about treatment. Despite opposing opinions, it is clinically proven that well-made and correctly set machine compression therapy helps hundreds of thousands of people.
It is important to make sure your device has adequate capabilities and that you use it correctly! This is not complicated. On my blog you will find more articles and videos on the topic.
Can machine lymphatic drainage be used on children?
Compression devices are not recommended for infants and children under 6 years old. General decongestive therapy (bandaging, compression stockings, manual lymph drainage combination) is preferred.
How important is the pressure gradient?
Devices that allow setting a pressure gradient prove to be the most suitable for reducing lymphedema. Your device is not ineffective just because it does not provide a pressure gradient, but it is less effective than ones that do.
What is machine treatment comparable to?
Unlike the circulatory system, the lymphatic system has no built-in motor. In the blood vessels the heart pumps blood. The lymphatic system relies on muscles — their contractions keep lymph moving. When a muscle contracts, it compresses a lymphatic vessel and lymph is pushed upward. Alternating compression by the device imitates this natural muscle pump function of lymph circulation.
I don’t move at night. How can lymph flow then?
Your muscles are regulated by the brain. A few percent of your muscle fibers remain active even during deep sleep and perform tiny contractions. You don’t feel or see these twitches, but they are enough to maintain lymph and partly blood flow. So flow does not stop even during sleep.
How should I set the appropriate treatment pressure for lymphedema?
Measuring your blood pressure can give a good guide. If your blood pressure is 120/80 mmHg, the 120 is the pressure when your heart contracts and pumps blood into the arteries. The 80 is the pressure when your heart rests between beats.
Treatment pressure should NEVER be set higher than the lower (diastolic) value! In fact, you should set it at least 20–30% below this value. So with 120/80, set maximum pressure in the lower airchamber to about 55–65 mmHg and decrease toward the thigh/upper arm.
Some therapists prefer even lower pressures on the arm (maximum 40–50 mmHg).
High pressure moves a lot of fluid suddenly and overloads the tissues above. Regular use of high pressure can worsen your condition over time. Higher pressure is therefore not better.
There are cases, such as fibrosis, where firmer tissues may require higher pressure to soften them. In severe fibrotic conditions, pressure treatment must be conducted under the supervision of an experienced therapist.
How long should I use the device daily?
If you have time for only one session a day, do it in the evening before bed. You may have noticed that in the morning the edema is significantly less (while you sleep some fluid drains from the limb).
If possible, split the treatment into two sessions: one in early afternoon and one in the evening.
A session can last from 20 minutes up to an hour depending on the desired outcome. Lower pressure requires longer sessions. For most people half an hour to, at most, two hours daily is sufficient. Longer treatments should only be done on a therapist’s recommendation.
Splitting treatment into multiple sessions is better because it reduces fluctuations in swelling. If you wait too long and swelling is high, reduction becomes more difficult. More frequent treatment prevents excessive filling.
Every case is different and requires individualized treatment. Only change therapy if your lymphedema therapist recommends it.
Can I use the compression therapy unit with ulcers and open wounds?
A compression therapy unit can be used with venous ulcers or open skin wounds if there is no infection and no signs of cellulitis. The wound or ulcer itself must be covered (with wound dressing) during treatment. The treatment cuff must be cleaned and disinfected after use.
Active skin infection or inflammation (e.g., erysipelas) is a contraindication because pressure could spread the pathogens or push them into the bloodstream, causing systemic infection.
Signs of active infection: local swelling, pain, redness, purulent discharge, red streaks on the skin. If any of these signs are present, do not use the pump and see a doctor immediately. Infection requires antibiotic treatment.
I have lymphedema and a leg ulcer and my doctor forbids using the compression therapy unit. Why?
Probably the doctor did not think the restriction through or does not understand what a compression device does.
Lymphedema makes the leg tight and this causes severe circulatory impairment. Slow circulation means wounds on an edematous leg easily become infected and are very slow to heal.
If the tense edema is not reduced — which is what machine therapy does — healing cannot be expected because poor circulation is the cause.
Therefore, in the case of an ulcer, healing can be achieved by improving circulation and reducing tension — that is, by machine therapy.
I had a compression treatment at my beautician and my leg hardened and became painful afterwards. What caused this?
A beautician is not authorized to treat lymphatic disease, but that is the lesser problem. The larger problem is when they do not know what they are doing. Post-treatment pain and hardening indicate treatment with inappropriate (too high) pressure.
A single poorly performed session is unlikely to cause permanent damage. However, if you regularly receive such treatments, your condition can deteriorate quickly and may become untreatable within months.
See a qualified specialist!
I had a compression treatment at my beautician and my varicose veins became inflamed and painful. What caused this?
Pain and “inflammation” of the veins indicate treatment was done with too high pressure and insufficient care. Your enlarged, twisted veins were roughly massaged by the device. Ice the area for 2–3 days and avoid strenuous activity (no workouts, but walking is allowed). Until superficial phlebitis resolves, do not have further machine or manual massage.
Instead of an unqualified beautician, consult a lymphedema therapist!
I developed a headache during machine treatment! What caused it?
This results from excessively high treatment pressure or treating too large an area at once (e.g., both legs and trunk). This pushes blood out of your legs and even trunk, raising your blood pressure. Headache is only the first sign! If excessive-pressure treatments continue, they can cause chest tightness and shortness of breath, and in extreme cases even cardiac arrest. Yes — incorrect use of a compression therapy unit can be fatal.
Find a treatment center that pays better attention to proper settings. If you feel a headache during treatment, stop the session and inform the operator immediately.
High blood pressure is not an absolute contraindication to machine therapy, but you must use even lower-than-usual pressure and reduce the treated area. Treat one leg at a time, then the other, and finally the trunk. This means three separate sessions — three times the duration — but avoids adverse effects.