Causes and Treatment Options of Peripheral Neuropathy
Peripheral neuropathy is damage to the peripheral nerve fibers, which causes sensory and balance disturbances and unsteadiness. Its main symptoms are tingling, numbness, burning sensations and a feeling of vibration. Pain often worsens at night, and touching the painful area or even changes in temperature can increase it. Neuropathy is not yet curable. Symptom relief is limited but possible.
Peripheral neuropathy
Peripheral neuropathy is a type of damage to the peripheral nervous system. It affects the nerves that transmit information from the brain and spinal cord (the central nervous system) to the rest of the body and back.
Neuropathy most commonly results from diabetes, autoimmune diseases, or alcoholism. It can also be a frequent side effect of chemotherapy and radiation therapy. Some forms are hereditary, while others develop due to injury.
There are more than 100 types of peripheral neuropathy, each with its own symptoms and prognosis. They are classified into the following categories:
- Motor neuropathy. Damage to the nerves that control muscles and movement of the body, for example moving the hands and arms or speech.
- Sensory neuropathy. Sensory nerves transmit signals of pain, temperature, or touch.
- Autonomic neuropathy. Nerves that control functions you cannot voluntarily influence, such as breathing and heartbeat.
- Combined neuropathies. Two or three of the above types may be present at the same time. An example is sensorimotor neuropathy.
Symptoms of peripheral neuropathy
Symptoms depend on which type you have and which part of the body is affected. They can range from tingling or numbness in a specific body part to more severe effects such as burning pain or paralysis.
- Burning, tingling pain, numbness, a "stinging nettle" sensation
- Muscle weakness, cramps, muscle twitches, loss of muscle mass (atrophy)
- Loss of bone mass
- Changes in the skin, hair, or nails
- Loss of sensation or feeling in body parts
- Loss of balance as a consequence of losing sensation in the legs, arms, or other body parts
- Emotional disturbances
- Sleep disorders
- Loss of pain sensation. This can be dangerous, for example you may not notice when you're injured.
- Inability to sweat, causing heat sensitivity
- Loss of bladder control, which can lead to recurrent infections or incontinence
- Dizziness, lightheadedness, or fainting due to loss of blood pressure regulation
- Diarrhea, constipation, or fecal incontinence related to nerve damage in the intestines or digestive system
- Difficulty eating or swallowing
- Life-threatening symptoms, such as difficulty breathing or irregular heartbeat
Treatment of peripheral neuropathy
The symptoms of peripheral neuropathy can resemble other diseases or medical problems. Therefore, making an accurate diagnosis is very important. In many cases neuropathy is related to an underlying disease, so your managing physician may already expect its appearance. If no such condition is known, a thorough workup may be necessary. See a neurologist!
Peripheral neuropathy is generally not curable, but its progression can be prevented. If your underlying disease is, for example, diabetes, then that must be treated first. Pain and other neuropathy symptoms are addressed afterward.
Medications sometimes help and sometimes they don't. This applies to both over-the-counter pain relievers and prescription drugs. The fact that one tried medication doesn't work doesn't mean another won't. It often requires "trial and error." In extreme cases, surgery may be used to destroy nerves that cause neuropathic pain and symptoms — of course only after all conservative methods have failed.
Prevention is the most effective method
Lifestyle choices play a role in preventing peripheral neuropathy.
You can reduce the risk by avoiding alcohol, correcting vitamin deficiencies, eating a healthy diet, losing weight, avoiding toxins, and exercising regularly.
If you have kidney disease, diabetes, or other chronic health problems, lifestyle measures are especially important: they can delay or even completely prevent peripheral neuropathy from developing as a complication.
Treating peripheral neuropathy
If neuropathy is already bothering you in some form, switching to a healthy lifestyle can help reduce the pain and symptoms associated with the condition. You should also quit smoking. Pay close attention to treating any wounds or injuries.
TENS treatment and neuropathy
In Germany, doctors almost always recommend TENS treatment. In other countries, including ours, it is not as well known or popular for this purpose.
TENS is a pain relief procedure, i.e. it provides symptomatic treatment and does not repair the damaged nerves.
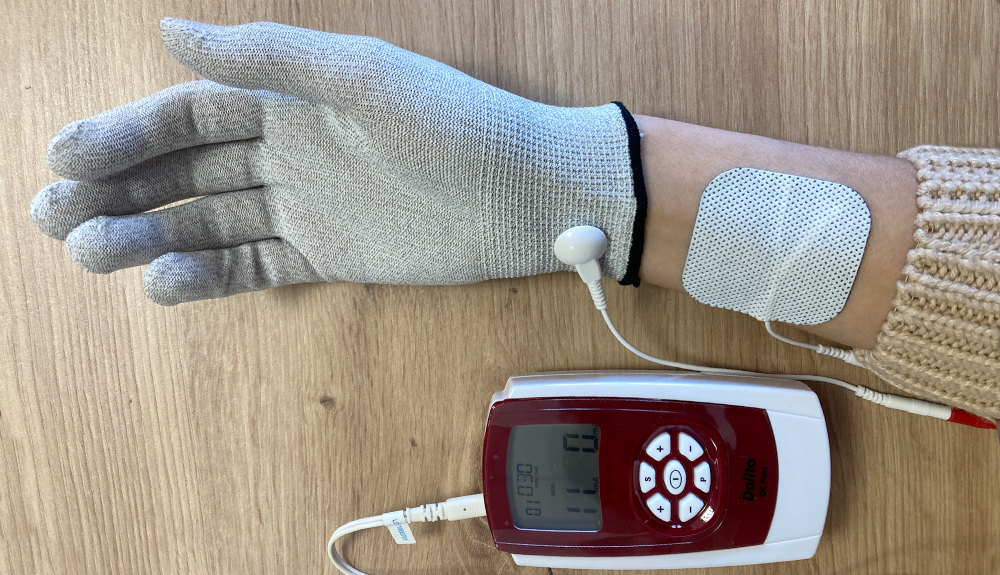
For neuropathy treatment, pull the glove electrode onto your hand. You can use it dry, but the treatment may be more effective if you moisten it. Dip the glove into lukewarm water and squeeze out the water so it does not drip. Put it on while damp.
Stick one electrode above your wrist. Leave 3–5 cm distance between the edge of the glove and the electrode.
Connect the cable to the device. Attach the positive (red) cable end to the glove and the negative (black) end to the self-adhesive electrode.
On the Dolito device start program 1 and increase the intensity.
Warning! Severe neuropathy means that the sensory nerve endings in your hands and feet are damaged, so you may not feel the pricking of the electric current.
Generally 8–18 mA is sufficient! Current above 30 mA may even cause skin burns (which you might not feel because of the neuropathy!).
The same application method may also help reduce the pain of rheumatic small-joint inflammation.
In the video below I use the Dolito device, but any TENS device can be suitable for the task.
Softlaser and neuropathy
One possible way to reduce neuropathic pain is softlaser treatment. Click here to read about the scientific evidence.
This is also a symptomatic therapy that takes advantage of the fact that laser radiation can reduce pain.
The laser treatment should be performed on the area affected by pain, moving point by point. The duration of the treatment depends on the device's power, the laser beam diameter, and the size of the area to be treated.
Laser treatment should be performed once daily. The Personal Laser L400 softlaser may be suitable for this purpose.
Click here to read more about softlaser treatment.
BEMER treatment and neuropathy
Another method for treating neuropathic complaints is Bemer therapy (click here to read more about it).
The method significantly improves microcirculation (i.e., circulation in the small vessels). This increases the amount of blood reaching the tissues, delivering vital oxygen and nutrients while removing harmful substances, metabolic waste, and toxins. The device is not cheap. Those who can afford it will not only reduce neuropathy symptoms but also benefit for any conditions caused by impaired blood circulation.
PEMF (pulsed electromagnetic field) treatment and neuropathy
Pulsed electromagnetic field (PEMF) therapy can also be used in polyneuropathy and may produce beneficial effects.
PEMF therapy can help restore the electrical potential of cell membranes, which promotes healthy cell function and improves the cells' regenerative capacity. The anti-inflammatory effect of magnetic field therapy is proven, which is important in polyneuropathy because inflammatory processes may underlie nerve damage. By reducing inflammation, PEMF also reduces inflammation-related pain. PEMF improves microcirculation, which enhances tissue oxygen and nutrient supply, speeds removal of metabolic waste products, and thereby supports regenerative processes.
A PEMF therapeutic device suitable for neuropathy treatment should have general tissue regeneration or general anti-inflammatory protocols. For example, Magnum 2500, Magnum XL Pro, Magnum 3000 Pro.
Muscle stimulation and neuropathy
Muscle atrophy (medically called atrophy) can be a consequence (complication) of peripheral neuropathy. Muscles lose mass (the circumference of the limb decreases). At the same time, muscle strength also decreases.
Sensory disturbance can affect joint position sense (proprioceptive) receptors, resulting in an unsteady, stumbling gait. This can lead to reduced movement, which accelerates deterioration of the condition, making movement increasingly strenuous.
The most effective method to prevent loss of muscle strength is regular exercise, such as a minimum 30–40 minute walk or cycling. If you cannot do these, use a muscle stimulator. This does not replace exercise but helps slow down and stop loss of muscle strength, and with appropriate frequency and duration can even help regain muscle strength.
Click here to buy a muscle stimulator device.
In this article I describe for example the program that helps restore thigh muscle strength and the devices with which it can be carried out.
Relaxation, meditation, yoga
Relaxation techniques can help relieve emotional and physical symptoms.