Fecal incontinence refers to the partial or total loss of control over bowel movements. It can manifest as involuntary stool passage or an urgent need to defecate that cannot be resisted. The severity of the condition varies from occasional mild symptoms to daily, severe cases.
Anatomical Background and Functional Mechanism
Control of defecation is a complex process requiring the coordinated action of multiple muscles and nerves. The anal sphincter consists of two parts: an external muscle controlled voluntarily and an internal muscle that functions automatically. Additionally, proper functioning of the pelvic floor muscles and rectal walls is essential for normal bowel movements.
Causes of Fecal Incontinence
There are numerous causes behind fecal incontinence.
One of the most common causes is the condition following anal surgeries, especially after hemorrhoid or rectal cancer operations. Injuries sustained during childbirth occur in women, while prostate surgeries may cause similar problems in men.
Neurological diseases such as multiple sclerosis, spinal cord injuries, or stroke can also lead to fecal incontinence.
Advancing age, weakening of the sphincter muscles, and nervous system dysfunctions increase the incidence of this problem.
Diagnostic Options
Exact diagnosis is necessary to choose the appropriate treatment. Medical examination includes a detailed medical history focusing on symptom characteristics, frequency, and triggers. Physical examination assesses the anatomical conditions around the anus and the functioning of the sphincter muscles.
Additional tests may include anal manometry, which measures sphincter pressure, and various imaging methods (ultrasound, MRI) helping to detect anatomical abnormalities.
Conservative Treatment Options
The first step in treatment is usually conservative therapy.
Pelvic floor muscle training plays a key role in rehabilitation. These exercises can be learned with physiotherapist support, and regular practice can significantly improve symptoms.
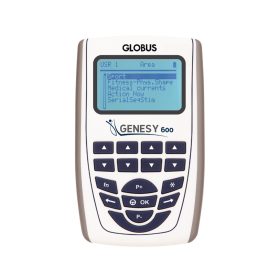
Pelvic floor exercises can be supplemented and made more effective by using incontinence stimulators.
Biofeedback therapy provides visual or auditory feedback on muscle activity via special devices, helping to learn proper muscle function. This method can be especially effective in postoperative rehabilitation.
Role of Lifestyle Changes
Lifestyle modification can greatly improve symptoms. Regulating stool consistency through proper diet and hydration is crucial. Optimizing fiber intake and regular meals can help establish a predictable bowel routine.
Normalizing body weight is also important since overweight increases intra-abdominal pressure and can worsen pelvic floor muscle function. Regular exercise, particularly targeted abdominal and pelvic floor workouts, can improve the condition.
Medication Options
Medication aims to regulate stool consistency or influence bowel movements. Anti-diarrheal medications can be used in cases of diarrhea, while appropriately chosen laxatives may help develop regular bowel movements in constipation cases.
In some cases, imbalance in intestinal flora may underlie the problem, where the use of probiotics can be considered.
Surgical Solutions
When conservative treatment does not yield satisfactory results, surgery may become necessary. The type of surgery depends on the cause and severity of the problem. Sphincter repair surgery can be performed if there is an anatomical injury.
In more severe cases or after repeated surgeries, artificial sphincter implantation or sacral nerve stimulation (SNS) might be options, the latter using electrical impulses to stimulate nerves controlling pelvic floor muscles.
Importance of Psychological Support
Fecal incontinence can cause significant psychological burden and negatively affect self-esteem and social relationships. Psychological support can help cope with these difficulties and improve quality of life.
Support groups or peer communities also offer valuable assistance by providing opportunities to share experiences and receive practical advice.
Everyday Life Advice
Organizing daily life is crucial for those living with fecal incontinence. It is recommended to always carry hygiene items and spare clothing. Various protective creams and cleansing products are available to protect the skin.
Proper arrangement of workplace and home, such as easy access to toilets, is also important. Before long travels, it is advisable to thoroughly plan the route and rest stops.
Therapeutic options for fecal incontinence continue to evolve. Early recognition and consulting the appropriate specialist are key to successful treatment. Generally, this is a manageable condition, and significant improvement can be achieved with proper therapy.